
October 2, 2025
Whole Person Care (WPC) requires a robust digital backbone to connect clinical, behavioral, and social care securely and efficiently. The hidden heroes? FHIR, computable consent, and AI-ready data.
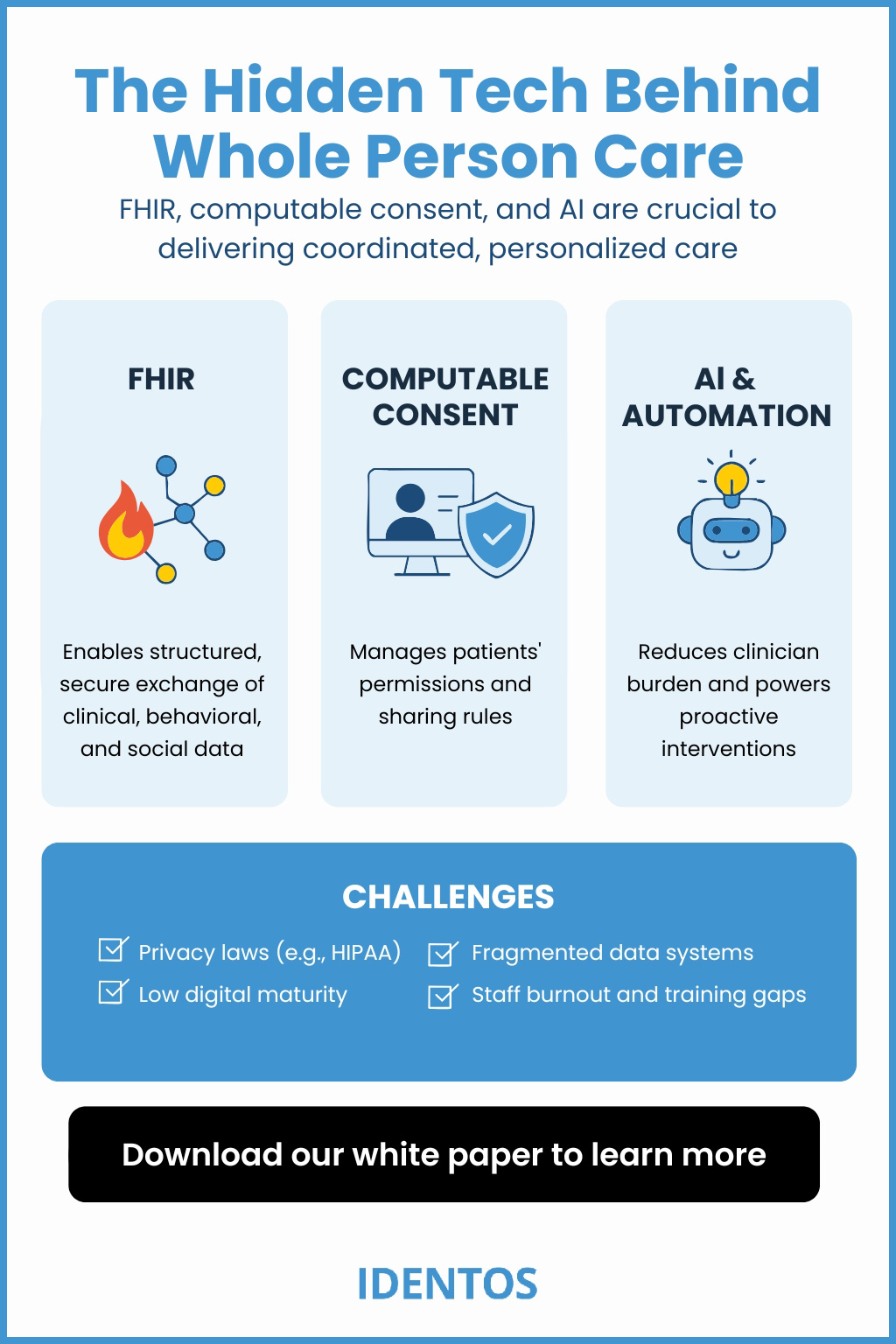
To deliver coordinated, personalized care, health systems must overcome data silos, privacy concerns, and legacy systems. That’s where the following three pillars come in:
FHIR (Fast Healthcare Interoperability Resources) is the global standard for securely exchanging health information across systems. It allows:
Example:
California’s Care Everywhere platform and Chicago’s Consent Service Utility both use FHIR to connect data from multiple sources.
What is computable consent?
It’s a digital framework that captures and enforces a person’s permissions for how their sensitive data is shared. The most advanced version of computable consent is currently under development by HL7 FHIR and is in a trial-use phase. This is critical when dealing with:
Why It Matters:
Example:
The Cook County CIE used a FHIR-based Consent Service Utility that allowed patients to control which parts of their record could be shared across housing, healthcare, and behavioral systems.
AI tools power the shift from episodic treatment to preventive, personalized care by:
Example:
The United States Department of Veterans Affairs (VA)’s Whole Health System used AI to tailor personal health plans aligned with veterans’ life goals, helping save $4,500+ per veteran annually.
Technology & Role in WPC
Together, they create a scalable digital ecosystem that supports holistic, human-centered care.
Q: Is FHIR secure enough for sensitive health data?
Yes. FHIR is built with secure authorization and access layers and supports granular sharing preferences when used with computable consent tools.
Q: How is AI used without violating HIPAA?
AI can be deployed using federated learning, which trains algorithms on local data without moving it, preserving privacy.
Q: What is computable consent vs. written consent?
Computable consent is machine-readable and enforceable in real-time, enabling systems to automatically comply with patient preferences.
Technology Makes Whole Person Care Possible
WPC isn't just a philosophy; it’s a system that requires standards, infrastructure, and trust. FHIR enables interoperability. Consent enforces ethics. AI fuels smart, proactive decisions.
Without these tools, whole person care remains an ideal. With them, it becomes a reality.
Want to Explore Consent-Centric Infrastructure for Whole Person Care?
Download our white paper or contact IDENTOS to learn how we enable ethical, scalable WPC systems with FHIR and consent at the core.
• What is Whole Person Care and Why is it the Future of Healthcare?
• How the VA Saved $4,500 Per Veteran with Whole Health
• Why Affordable Housing is a Health Priority, Not Just a Policy Issue
If you have any questions or require further information regarding this topic, please don’t hesitate to contact us using the form below.